Hematologist
Higher education:
Hematologist
Samara State Medical University (SamSMU, KMI)
Level of education - Specialist
1993-1999
Additional education:
"Hematology"
Russian Medical Academy of Postgraduate Education
Statistics show that a tenth of the patients of the surgical department are hospitalized with bleeding of the gastrointestinal tract. Usually patients are delivered by an ambulance team, less often they come from the therapeutic department. Treatment often consists of therapy for the underlying pathology and measures to replenish lost blood. The operation is indicated for serious problems with the intestines (vascular ischemia, thrombosis, tissue death).
Gastrointestinal bleeding
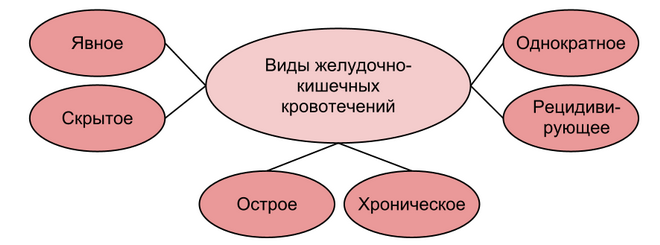
Experts attribute gastrointestinal bleeding (GI) to the negative consequences of certain diseases that threaten the health and life of the patient. Blood loss can reach up to four liters, and therefore require urgent medical attention. Bleeding from the intestines is divided according to:
- with the causes of development (ulcerative, non-ulcerative);
- with the nature of blood loss (acute, chronic);
- with symptoms (obvious, hidden);
- manifestations over time (single, recurrent).
Causes of intestinal bleeding
The causes of intestinal bleeding are varied:

Intestinal bleeding is often caused by vascular lesions (sclerosis, thrombosis, ruptures) and disturbances in the body's reactions to prevent and stop blood loss. Often these factors appear at the same time. Blood loss in gastric ulcers and the initial section of the small intestine usually occurs during exacerbation of chronic pathology and is provoked by purulent fusion of the vessel wall. Sometimes the outflow of blood from the rectum is observed after prolonged constipation. In infants, bleeding is possible due to volvulus, in older children - due to the formation of polyps in the colon.
Manifestations of intestinal bleeding
The localization of blood loss affects the manifestations of gastrointestinal bleeding. The most obvious symptoms of intestinal bleeding are blood in the stool and vomit. Scarlet blood appears in vomiting when blood flows from erosions, varicose esophageal veins and from the stomach. She gets a brown tint after a reaction with hydrochloric acid during ulcerative bleeding and in Mallory-Weiss pathology. The blood in the feces is also not changed - with momentary ulcerative bleeding of more than 100 ml or with the outflow of blood from the lower parts of the digestive tract. With prolonged gastrointestinal bleeding from the upper sections of the feces, black, tarry. Sometimes this is the only sign of a non-obvious ulcerative bleeding. If blood is excreted from the small intestine, stomach, or first sections of the large intestine, it is usually evenly distributed in the stool. Bleeding in the rectum is characterized by bloody clots in normal stools. Tumors of the rectum provoke false urge to defecate. In addition to the appearance of blood in the feces and vomiting, there are other signs of bleeding from the intestines:
- dizziness;
- muscle weakness;
- "flies" and a veil in the eyes;
- sticky sweat;
- pallor.

Signs depend on the massiveness of blood loss and range from slight weakness to coma. But the risk of opening intestinal bleeding does not exclude even the absence of general symptoms.
Varicose veins of the digestive tract
The esophagus passes into the stomach, forming a plexus of veins. The portal vein, which takes blood from the intestine, converges with the superior vena cava, which contains blood from the upper body. The high pressure causes the veins to expand and injure themselves, causing bleeding.
At first, the patient does not notice the pathology - there are no obvious symptoms. Intestinal bleeding opens suddenly and is sometimes so massive that it leads to death.
Systemic vasculitis
Schönlein-Genoch purpura and periarteritis nodosa are autoimmune pathologies that affect the walls of blood vessels and increase their bleeding. Part of systemic vasculitis is manifested by the outflow of blood from the stomach. Signs of blood loss appear simultaneously with the symptoms of the underlying pathology.
atherosclerosis, high blood pressure
High blood pressure in vessels affected by atherosclerosis increases the risk of rupture of their walls during injury or a sudden change in pressure. Under such circumstances, intestinal bleeding is inevitable. Before gastric effusions, the characteristic signs of hypertension appear. Sometimes high blood pressure is asymptomatic.

Hemophilia
Hereditary pathology, characterized by poor blood clotting and bleeding. It appears exclusively in men. Intestinal bleeding in patients with hemophilia can cause the use of non-steroidal anti-inflammatory drugs, as well as exacerbation of peptic ulcers, erosive gastritis, hemorrhoids.
Blood effusions into the omentum and mesentery require differentiation from intestinal obstruction and acute appendicitis. Hemophilia is characterized by delayed blood loss - they do not appear immediately after the injury, sometimes after 12 or more hours.
Acute and chronic leukemias
Oncological diseases of the blood, which disrupt the processes of blood formation in the red bone marrow, negatively affect the formation of platelets, which are indispensable for blood clotting. In a quarter of patients, acute leukemia turns into a hemorrhagic form, manifested by severe blood loss, including from the digestive tract. Such leukemias progress extremely quickly - massive intestinal bleeding ends in death. Symptoms of bleeding, especially from the vessels of the gastrointestinal tract, are more often manifested in the chronic form of lymphocytic leukemia.
Hemorrhagic diathesis
A group of acquired and hereditary pathologies characterized by poor blood clotting and increased bleeding. Intestinal bleeding caused by hemorrhagic diathesis is observed infrequently, accounting for less than 1% of all acute gastrointestinal blood loss. They can provoke diseases:
- violating vascular permeability;
- negatively affecting the reactions of the body, helping to stop bleeding;
- anomalies of small blood vessels or their chronic pathologies.

Vitamin K deficiency
Vitamin K is essential for blood clotting. Its deficiency causes excessive bleeding, outpouring of blood into various organs, internal bleeding. The main causes of vitamin K deficiency are:
- low content in the food consumed;
- poor intestinal absorption;
- overexpenditure in hepatic pathologies.
To determine if there is enough vitamin K in the body, you need to pinch yourself in the back of the hand and pull back the skin. In this state, count to 60. A bruise or noticeable redness that appears at the site of exposure indicates a vitamin K deficiency.
Hypoprothrombinemia
A variety of substances are involved in the process of blood coagulation, including prothrombin. Its deficiency in the blood is congenital and acquired. In a patient with a diagnosis of "hypothrombinemia", bleeding is observed only in the case of a significant decrease in the level of prothrombin. Then bruises appear on the patient's body, unexplained bleeding, including intestinal bleeding, opens.
From bleeding under such circumstances, virus-inactivated concentrates of the prothrombin complex help. In case of injuries and operations, such a patient is under medical supervision. Therapy and prophylaxis can be carried out using frozen plasma.
Diagnosis of stomach bleeding
Symptoms of intestinal bleeding are similar to nasopharyngeal bleeding - when swallowed, it can enter the gastrointestinal tract. In addition, blood in the respiratory tract sometimes enters the process of vomiting. In such cases, a differentiated diagnosis is necessary. Massive bleeding from the esophagus should be differentiated from necrosis of the heart muscle. Vomiting is observed exclusively with blood loss, pain in the chest area is inherent in a heart attack. If a woman is of reproductive age, blood loss during an ectopic pregnancy should be excluded.

Standard diagnostic methods for intestinal bleeding:
- collection of anamnesis;
- physical examination and rectal-finger examination of the rectum;
- hemostasiogram and clinical blood test;
- study of feces;
- instrumental studies (main - endoscopy).
Therapy for intestinal bleeding
Treatment of intestinal bleeding includes:
- providing bed rest for the patient, excluding psycho-emotional and physical stress;
- clarification of the causes of blood loss;
- replenishment of lost blood by intravenous infusions of solutions that replace blood; with a significant loss of blood - by transfusion of donor blood and its components;
- the use of blood-stopping drugs and iron-containing drugs (to eliminate anemia);
- surgical manipulations.
With heavy and repeated bleeding, surgical therapy often remains the last resort for saving the patient. An urgent operation is indicated when the ulcer is perforated and it is impossible to stop blood loss with medications, including when blood flows from the rectum. Surgical intervention is usually carried out at the initial phases of blood loss - the results of late operations are less favorable.
First aid for intestinal bleeding
If esophageal bleeding is suspected, an emergency team should be called. Prior to her arrival, the following steps must be taken:
- lay the patient down, raising his legs;
- exclude the use of food and liquid;
- place an ice pack or other chilled object in the area of bleeding;
- give a hemostatic agent (Dicinon).
Do not attempt to wash the stomach and apply an enema. When bleeding from the rectum, you should not even sit - this will cause blood flow to the veins of the pelvis and intensify the phenomenon. If the patient has lost consciousness, ammonia can be used. Before the arrival of the doctor, it is necessary to monitor his breathing and heartbeat.
Rehabilitation after gastric bleeding
After suffering blood loss, the patient fasts for a couple of days, nutrients are injected into him intravenously. Then raw eggs, milk, fruit jelly are included in his diet. A week later, it is allowed to use cottage cheese, grated cereals, soft-boiled eggs, meat soufflé, jelly.
After blood loss, time is needed to restore the structures of the affected organs and heal the lesions. A strict diet should be followed for at least six months. At this time, any physical activity is prohibited.
Six months later, the patient needs to be examined again and continue to follow all the recommendations of the gastroenterologist. The question of the advisability of spa treatment should be agreed with the doctor.
It is difficult to make predictions about the outcomes of intestinal bleeding - it is influenced by a variety of factors. Mortality from bleeding from the gastrointestinal tract at all times is quite high. The most important thing is to identify the pathology leading to blood loss in time and strike a preemptive blow by organizing adequate treatment.



